Brain Cancer Databank
Brain Cancer Databank
Brain Cancer DataBank Concept
Introduction
The comprehensive DataBank will comprise data from three linked projects under TBCG. Conceptually once established every patient will be entered into the TBCG Brain Cancer DataBank through a linked pathway in which their initial brain tumour specimen is stored, alongside their actual brain cancer images and their information data. A scientist asking a question can then access the actual brain tumour specimen, and see how that influences the MRI appearance and treatment outcomes. It will be a powerful future resource for the Brain Cancer community.
1. Brain Tumour BioBank and Laboratory
This is the Laboratory situated in the Kolling Institute of Medical Research on the Royal North Shore Hospital campus and contains the biological samples of patients brain tumours, as well as the biological research laboratory studying the tumour specimens. Funding for this laboratory has been from previous fundraising campaigns and is now an established unit.
2. Clinical Outcomes Database
This is the detailed database that gathers baseline tumour and treatment information from our patients and assesses the outcomes of treatment. This is being funded by a donation from the family of Tim Cohen. Information from the BioBank and Imaging Laboratory will feed into this database.
3. Brain Cancer Imaging Laboratory
This is new imaging databank under development paralleling the principles of the Brain Tumour BioBank and Laboratory gathering the actual images from patients for future study and assessment. It will be the only Imaging Laboratory in Australia and be a great resource for local and international researchers.
TBCG Brain Imaging Laboratory
What is it?
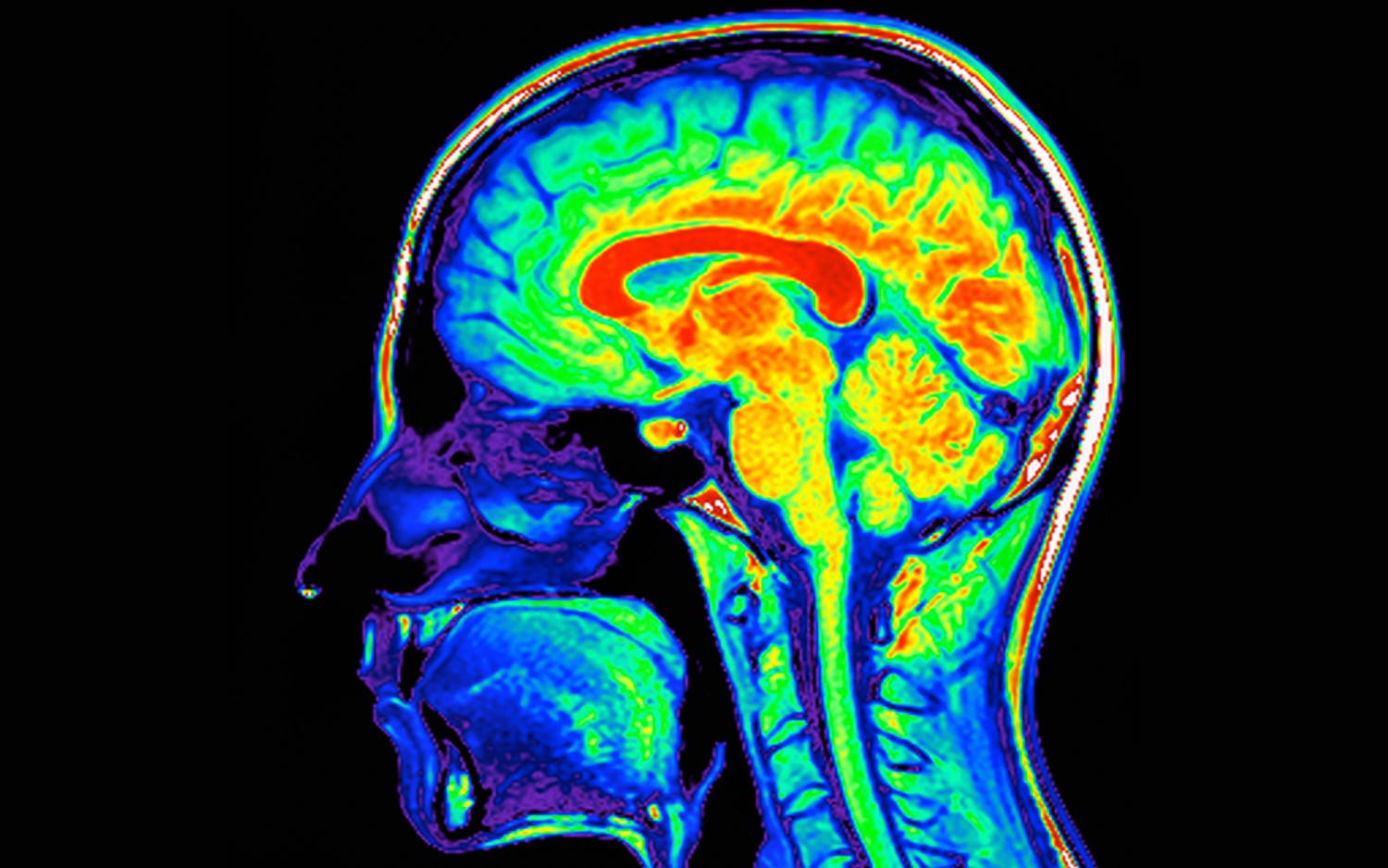
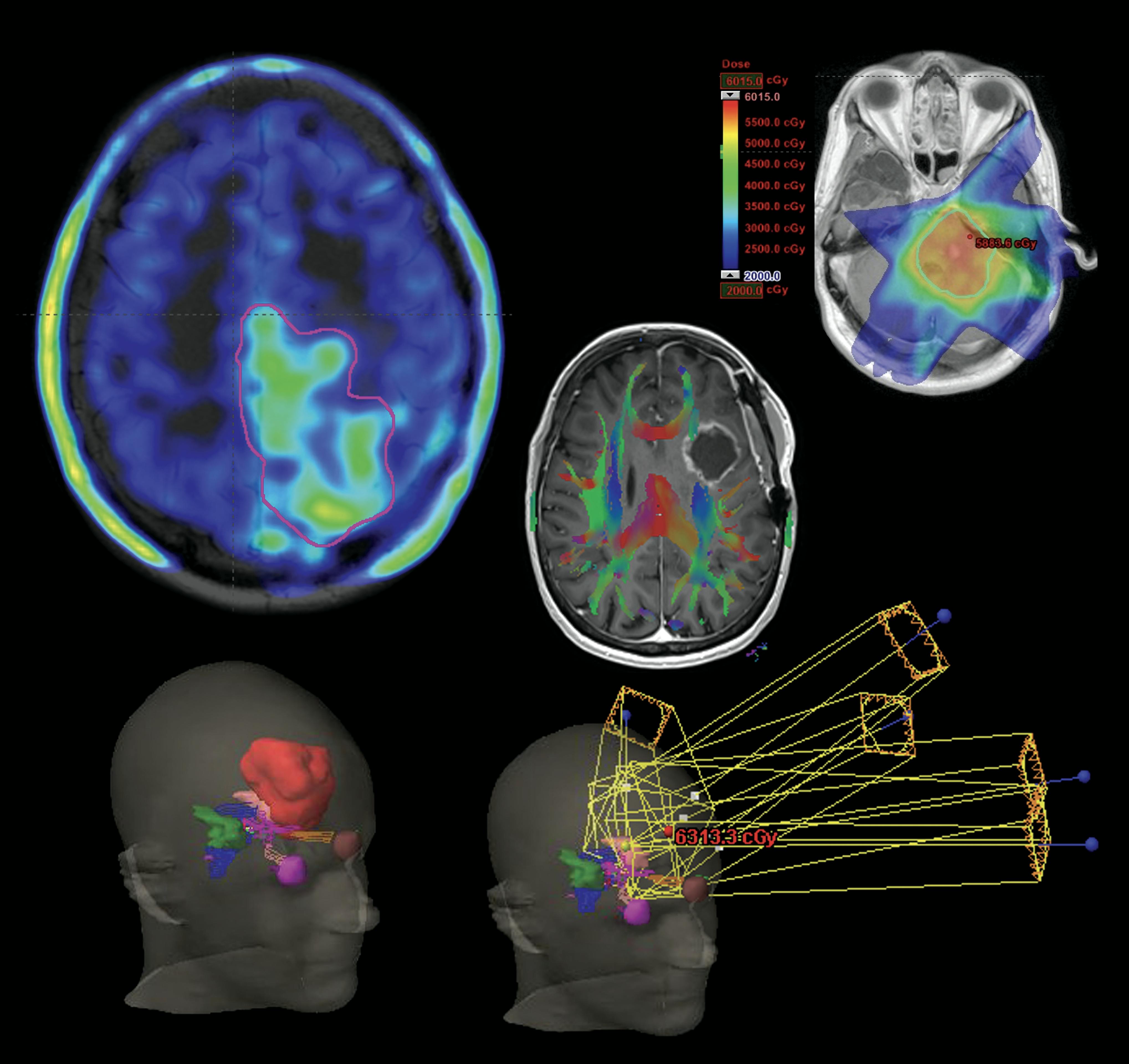
Current treatment for brain cancer aims either to directly destroy the tumour (neurosurgery and radiation therapy) or change the ways that the cancer can grow within the brain (chemotherapy or immunotherapy). Whilst a lot of laboratory research both in The Brain Cancer Group (TBCG) and internationally is directed at working out the way the cancer can grow, there is less research at targeting exactly where the tumour is situated or hiding within the brain. This unfortunately means that the current methods of X-ray imaging (MRI scans and PET scans) limit the ability for the neurosurgeon or radiation oncologist to target the cancer.
TBCG is developing a Brain Cancer Imaging Laboratory which will aim to improve the understanding and accuracy of these brain scans. It will gather and store the actual images from all our patient’s brain cancer imaging in one research databank; and then utilise this information from prior patients to understand where and how the tumours spread within the brain. Using sophisticated mathematical and artificial intelligence calculations, the research data from these brain scans can then be utilised to more accurately treat current and future patients with more precise targeted methods. In this way, the information from previously treated patients can be positively utilised for future patients, and hopefully lead to better brain cancer control and cure.
The Brain Cancer Imaging Laboratory will be the first of its kind in Australia and will collaborate with other clinicians, scientists and laboratories internationally. The Imaging Laboratory will link with the previously funded Brain Tumour Biobank and Clinical Outcomes Database to complete a powerful comprehensive TBCG Brain Cancer DataBank.
Context
Neuro-oncology management now has become increasingly dependent on imaging to guide decision-making both at time of diagnosis and post treatment evaluation.
More sophisticated imaging techniques have been developed to improve the mapping of a cancer; calculate a tumour's response to treatment or define the microstructure of tumour. Similar assessments can be performed on Nuclear Medicine PET imaging which enhances its utility as a decision-making tool, as well as novel radiotracers which can define biological aspects of tumour or treatment response. Deep learning analysis through Artificial Intelligence is a potential feature to get this information into the clinic.
Aim and scope
TBCG-BIL focusses on brain imaging research and radiology education in neuro-oncology. It takes a multimodality approach, harnessing novel imaging methods in both radiology with MRI and nuclear medicine with PET.
The research goals of the TBCG -BIL are fourfold:
- Improve diagnostic accuracy of imaging prior to surgery and chemoradiotherapy
- Offer new solutions to more accurately delineate the extent of disease by harnessing new imaging methods in MRI and PET
- Improve patient imaging experience with accelerated imaging protocols
- Improve clinical outcomes and survival by leveraging these novel imaging methods to predict patterns of recurrence, offer personalised adaptive radiotherapy plans and improve treatment effectiveness.
The laboratory also provides education both internally within medical multidisciplinary teams but also more broadly to our referring clinicians and our brain cancer patients and their families. TBCG-BIL also explores a neuro-imaging research focus in neuro-inflammation, demyelination and neurovascular imaging, which indirectly may provide clues into brain cancer.
With our research partners the TBCG-BIL has access to state-of-the-art imaging equipment on the North Shore campus including 5x MRI scanners, 2x PET scanners as well as Interventional Neuroradiology, PET radiochemistry and neuro-nuclear therapies.
“The TBCG Brain Imaging Laboratory will challenge what we know about brain cancers and help to transform the management of this unrelenting disease.”

Associate Professor Michael Back
TBCG-BIL Research Projects
Aim:
Image newly diagnosed GBM patients with ‘hypoxia’ / ‘oxygen enhanced’ imaging methods on both MRI and PET to delineate regions of radiotherapy resistant disease. 3 yr timeline: recruitment starts Q1 2022.
Description:
Prospective study ~20 patient recruitment with multiple scans over the course of therapy. Partnership with ACRF Image X Institute, USyd, North Shore Radiology and Siemens.
PI: Drummond
AI: Brighi, Back, Waddington, Keall, Bailey
Aim:
Development of novel biophysical modelling in brain tumors using diffusion imaging. 2 yr timeline: recruitment starts Q4 2021
Description:
2x post-doc researchers. Later applied to brain imaging.
Partnership with USyd, NHMRC (outcome pending), UCL (London), UniSR (Italy).
PI: Bourne (USyd)
AI: Drummond, Panagiotaki (UCL)
Aim:
Implementation of automated postprocessing pipeline for advanced imaging analysis. Integration of multiple imaging tools to expedite and automate complex processing methods in MRI.
Description:
DSC / DCE perfusion
DTI methods – including decomposed p-mapping and cord DTI
Fusion methods and anatomical mapping
PI: Drummond
Implications for radiation therapy target volume delineation.
Aim:
This study aims to explore the pattern of infiltration and relapse in relation to adjacent white matter tract (WMTract) pathways.
Description:
Exploratory MRI volumetric study of >250 patients with glioblastoma managed 2016-2020. Diagnosis and relapse MRI re-assessed in relation to adjacent white matter pathways and neuroanatomical brain structures.
PI: Back
AI: Drummond, Jayamanne
TBCG-BIL Research outputs
10 year follow up of IDH mutant gliomas to assess the long-term MRI radiological abnormalities following high dose stereotactic radiotherapy
Date: Sept 2021
Journal/Venue: RANZCR
Output type: Oral Presentation
18F-FET-PET in the diagnosis and prognostication of primary brain tumours
Date: Sept 2021
Journal/Venue: RANZCR
Output type: Educational Exhibit
Self-Limiting Post radiotherapy enhancement events on MRI Surveillance following management for IDH-mutated Anaplastic Glioma
Date: Sept 2021
Journal/Venue: RANZCR
Output type: Scientific Exhibit
Influence of MRI T1/T2 ratio in predicting patient outcome at time of initial diagnosis of Glioblastoma
Date: Sept 2021
Journal/Venue: RANZCR
Output type: Oral Presentation
Recent Imaging Insight on Perivascular Spaces of the Brain
Date: Sept 2021
Journal/Venue: RANZCR
Output type: Poster Presentation
Patterns of infiltration and relapse of Glioblastoma involving the anterior temporal lobe: implications for radiation therapy target volume delineation and margin expansion.
Date: Sept 2021
Journal/Venue: RANZCR
Output type: Poster Presentation
Lu-DOTATATE in the treatment of recurrent meningioma
Date: Dec 2021
Journal/Venue: RSNA
Output type: Poster Presentation